Abstract
Background: Patients with colorectal cancer (CRC) are at increased risk of venous thromboembolism (VTE), but the precise mechanisms of hypercoagulability in CRC remain largely unknown. Neutrophil extracellular traps (NETs) are web-like chromatin structures decorated with cytoplasmic, granular and nuclear components of neutrophils, which can participate in both antimicrobial responses and contribute to a number of autoimmune and thrombotic diseases. However, a definitive role of NETs in the hypercoagulable state in CRC patients is still unclear. The aims of this study were to identify the novel role of NET in the induction of procoagulant activity (PCA) in CRC, and to evaluate its interactions with platelets and endothelial cells (ECs).
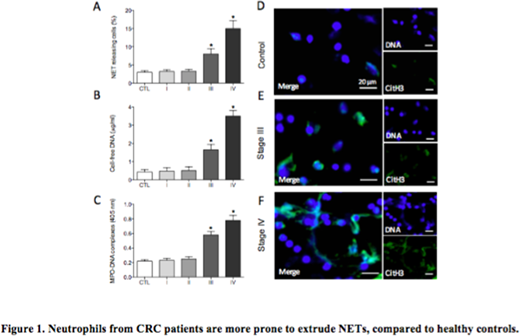
Methods: Ninety-two CRC patients and 30 healthy controls were included. The presence of NETs was assessed using immunofluorescence microscopy. Cell-free DNA (cf-DNA) was quantified using the Quant-iT PicoGreen dsDNA Assay Kit, myeloperoxidase (MPO)-DNA complex was measured using a capture enzyme linked immunosorbent assay (ELISA). Thrombin-antithrombin (TAT) complex of NETs was evaluated by ELISA. Coagulation time of NETs, platelets and ECs was assessed by coagulation time (CT) using one-stage recalcification time assays, purified coagulation complex and fibrin turbidity were measured using ELISA. PS exposure on platelets and ECs, and fibrin formation on ECs were detected with flow cytometry and confocal microscopy.
Results: We showed that the levels of cf-DNA and MPO-DNA complexes in the peripheral blood of CRC patients were increased in parallel with cancer progression and reached significance in stage III and IV patients compared to healthy subjects (all P<0.01). In addition, NETs released by CRC patients shortened coagulation time (CT), significantly enhanced the generation of TAT complexes and the formation of fibrin fibrils compared to healthy controls (all P<0.05). Moreover, DNase1-mediated degradation of NETs resulted in decreased PCA in patients with CRC (P<0.001). Furthermore, platelets from CRC patients stimulated healthy neutrophils to extrude NETs, which could be inhibited by the depletion of HMGB1 (P<0.01). Conversely, NETs from CRC patients could also induce the exposure of PS on platelets and the release of platelet MPs (PMPs), leading to markedly enhanced intrinsic/extrinsic FXa and FIIa, as well as shortened CT (all P<0.05). Importantly, endothelial cells (ECs) were converted to a procoagulant phenotype when exposed to NETs from CRC patients. The PCA of NETs-activated platelets or ECs could be inhibited either by the cleavage of NETs with DNase1 or the blockage of histone with activated protein C (APC) (all P<0.05). Our study also showed that the levels of NETs in CRC patients was positively correlated with TAT complexes and D-dimer (all P<0.05).
Conclusion: Our results suggest that activated platelets promote NETs formation through the release of HMGB1 and result in an elevated PCA in CRC patients. In turn, NETs induce platelet PS exposure and PMPs release, forming a vicious cycle. In addition, NETs could also induce a procoagulant phenotype of ECs, indicating the complex relationship among these cellular constituents and highlighting the procoagulant role and cytotoxic effects of NETs in CRC. We propose that the rapid developments in the field of NETs may provide new therapeutic targets to combat the thrombotic consequences of CRC.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal